Everything has changed in the modern world, from eating to sleeping patterns. So does the way your body reacts or responds. You must be aware of the stress hormones (Cortisol) secreted when your body experiences a stressful situation.
Now, imagine a situation where your body fails to respond to stress. It doesn’t mean that the stress hormone levels are deficient. It may have been caused by insufficient secretion of hormones that stimulate the synthesis of stress hormones. In this way, it has also become crucial to give importance to the stress hormone-releasing hormone just as we pay attention to the actual stress-responding hormones.
What is that crucial stress hormone-releasing hormone? It’s the adrenocorticotropic hormone (ACTH)!
Lately, many research pieces dealing with the sleep cycle have gained attention. Yes, your sleep-wake cycle is crucial in regulating adrenocorticotropic hormone secretion. Let’s see if current sleep-deprivation trends affect the synthesis and secretion of adrenocorticotropic hormone.
Adrenocorticotropic hormone
The adrenocorticotropic hormone is also known as Adrenocorticotrophin and corticotropin.
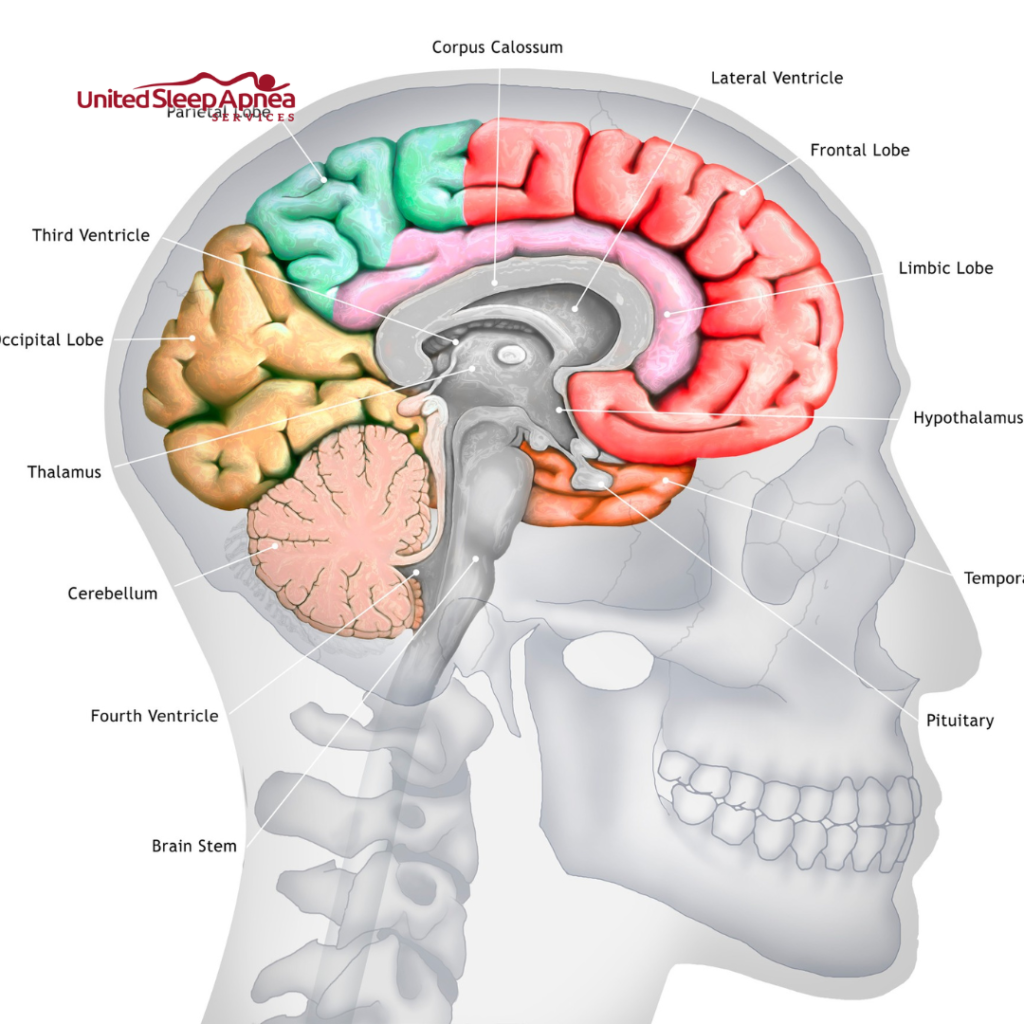
As the name suggests, the corticotroph cells located at the tiny pituitary gland‘s anterior part produce the adrenocorticotropic hormone. After reaching the bloodstream, this hormone reaches the adrenal gland, binds to its receptors in the cortex region, and stimulates the production of adrenal hormones (stress hormones).
The adrenocorticotropic hormone stimulates the adrenal gland to produce glucocorticoids (cortisol), mineralocorticoids, and androgens.
Synthesis and Secretion of ACTH Hormone
During stress, the brain’s hypothalamus secretes CRH (corticotropin-releasing hormone), which signals the pituitary to produce the adrenocorticotropic hormone. The pituitary produces the adrenocorticotropic hormone from the precursor protein Proopiomelanocortin (POMC).
Adrenocorticotropic hormone secretion occurs in a waveform pattern. Like cortisol, the adrenocorticotropic hormone is released in a pulsatile fashion in the morning. The secretion gradually drops throughout the day and reaches its lowest at midnight. This waveform resembles the circadian rhythm of your body.
Regulatory Mechanism
The hypothalamic–pituitary–adrenal (HPA) axis acts as the primary regulator for the adrenocorticotropic hormone’s secretion. Alteration in the functions of these three regions viz. Hypothalamus, Pituitary, and Adrenal greatly influence the synthesis of the adrenocorticotropic hormone.
Besides, a negative (feedback) loop mechanism regulates the adrenocorticotropic hormone levels in the bloodstream. When the cortisol levels in the blood increase, it inhibits the release of the corticotropin-releasing hormone by the hypothalamus, thus inhibiting the adrenocorticotropic hormone secretion by the pituitary gland.
A recent article (2019) on adrenocorticotropic hormone states that any stress (physical or psychological) may affect the cortisol levels and the adrenocorticotropic hormone levels.
Other brain regions that may affect the regulation of adrenocorticotropic hormone include the amygdala and prefrontal cortex. Apart from organs and hormones that regulate the adrenocorticotropic hormone, the body has neurotransmitters, peptides, and immune factors that play either a stimulatory or inhibitory role.
Functions of ACTH Hormone
The primary function of the adrenocorticotropic hormone is the stimulation of corticosteroid secretion. Other function includes:
- Increase of glucose oxidation
- Phosphate turnover
- Bone metabolism (Resorption)
- Immunosuppression
- Cholesterol consumption (Lipolysis)
- Genetic material synthesis (DNA/RNA)
- Protein catabolism
- Formation of muscles
- Spermatogenesis stimulation
Diseases associated with ACTH Hormone
The normal adrenocorticotropic hormone levels in your human body are 6.0 to 76 pg/ml or 1.3 to 16.7 pmol/L. However, there may be variations based on the age and sex of the individuals.
Primarily, the hypo- or hyper-function of the pituitary causes changes in the secretion of the adrenocorticotropic hormone. Abnormal adrenocorticotropic hormone levels may also arise due to stress, illness, endocrine disorders, and sleep disorders.
Excessive ACTH Hormone
The general symptoms of adrenocorticotropic hormone include acne, excess body and facial hair, pink stretch marks around the thighs or breasts, and fatigue.
Cushing's Disease
Non-cancerous adenoma in the pituitary leads to excess secretion of adrenocorticotropic hormone. This disease can be evoked at the adrenal and pituitary levels (tumor cells).
ACTH Hormone Deficiency
Hypopituitarism must contribute majorly to the deficiency of adrenocorticotropic hormone secretion. The general symptoms of adrenocorticotropic hormone deficiency include weight loss, hyperpigmentation, problems with women’s menstrual cycle, muscle or joint pain, frequent vomiting, low blood pressure, abdominal pain, and loss of appetite.

ARE YOU MISSING OUT ON THE MOST RESTORATIVE SLEEP OF YOUR LIFE?
Reduce your daytime fatigue with the latest diagnostic testing and physician services for improved health.
Our team of experts will listen to your concerns, guide you through the process, and answer all your questions.
How is Sleep associated with ACTH Hormone
The secretion of adrenocorticotropic hormone and cortisol follows the wave pattern of the circadian rhythm. An endogenous master pacemaker in the brain’s hypothalamus generates this circadian rhythm. Specifically, the hypothalamus’s suprachiasmatic nucleus (SCN) is responsible for the rhythm and works on day-light stimuli. When in light (illumination), your eyes send direct signals to the SCN, thereby regulating the wave pulse of the rhythm.
As per the HPA axis activity, the adrenocorticotropic hormone induces the adrenal gland to produce the stress hormone cortisol. Cortisol secretion follows the circadian rhythm, wherein the levels reach their lowest during nocturnal sleep (at midnight) and increase with wakefulness (early morning). The cortisol levels reach their highest at about 9 a.m. and slow down during the day (light). With the onset of sleep, again, the levels reach their lowest.
In general, the dysfunction of the HPA axis can affect your sleep quality, and at the same time, poor sleep or sleep fragmentation can affect the HPA activity.
Observational Studies
One of the sleep restriction studies on healthy subjects published in the Journal of Clinical Endocrinology and Metabolism found a strong association between sleep loss and adrenocorticotropic hormone.
The study observed around a 19% increase in adrenocorticotropic hormone levels during the day amongst the sleep-restricted subjects.
The study also analyzed the cortisol levels for sleep loss and found a significant increase. However, though the hormone levels increased, the pulse frequency remained unaltered for both adrenocorticotropic hormone and cortisol.

Researchers found an increase in the adrenocorticotropic hormone and cortisol levels, especially in the morning due to the HPA axis hyperactivity. Hence, the study claimed that sleep loss or restriction could only be a mild physiological factor affecting the HPA axis activity. As sleep restriction differently affected the levels of adrenocorticotropic hormone and cortisol, scientists claimed that sleep loss alters only the adrenals’ sensitivity to the secretion of ACTH.
This in-depth research also studied the involvement of CRH in activating the HPA axis activity and, thereby, the adrenocorticotropic hormone levels.
A similar study experimented with sleep restriction against the HPA axis activity and found significant HPA functioning changes following sleep loss. Sleep Journal research discovered that two nights of sleep restriction caused reduced recovery and loss of sensitivity in the HPA axis function.
Like the previous research, this study also analyzed the interference of corticotropin-releasing hormone. The study observed that the alterations in corticotropin-releasing hormone levels might have arisen due to reduced pituitary sensitivity. However, the study also claimed that this kind of HPA dysfunction might further increase the risk of sleep loss, leading to severe sleep apnea, obesity, diabetes, depression, and the onset of cardiovascular diseases.
As researchers carried out several studies to understand the association of sleep quality and the HPA axis, it paved the way to stronger evidence supporting the previous research and inconsistent results and observations over the years.
Acute Sleep Loss and HPA Axis
A study observed a biphasic HPA functioning pattern in response to sleep deprivation. The results published in the International Journal of Endocrinology say that several studies have observed increased cortisol levels due to consistent sleep deprivation (acute sleep loss patients), irrespective of the day or night. Hence, the findings supported high glucocorticoid levels among acute sleep loss patients.
Semi-chronic Partial Sleep Restriction
The HPA biphasic function research also found in chronic sleep-restricted patients that the glucocorticoid (cortisol) levels peaked in the morning and continued to peak even during the evening. Also, comparing chronic short and chronic long sleepers led to higher nocturnal glucocorticoid levels for chronic short sleepers than the other segment.
Insomnia
In insomniac patients, cortisol’s higher concentration increased throughout the day, including in the evening and nocturnal durations (sleeping time). However, this condition seemed slightly lower for those with less severe or persistent insomnia disorder.
Obstructive Sleep Apnea (OSA)
In general, several studies found an increased cortisol level among OSA patients. A research study published in the Journal of Respiratory Medicine studied untreated OSA patients and found no significant change in the secretion levels of pituitary hormones (here, adrenocorticotropic hormone) in response to sleep fragmentation due to OSA. However, the study showed increased cortisol levels, NE levels, and decreased thyroid-stimulating hormone levels.
Another observational study analyzed 72 subjects (male and female), studying their hormone levels for four continuous nights. The study revealed a significant increase in cortisol levels in both OSA men and women. Another study’s primary findings state that sleep apnea in middle-aged and non-obese men and slightly obese women significantly affects cortisol levels.
Regarding OSA’s effect on the HPA axis functioning, researchers investigated around 10 OSA patients, studying the association between sleep apnea and HPA dysfunction. The findings reveal that untreated OSA patients exhibit a strong relationship with HPA axis functioning and, in turn, the secretion of adrenocorticotropic hormone and cortisol.
Among these subjects, the study also found the influence of hypothalamic corticotropin-releasing hormone (CRH) and arginine vasopressin (AVP) that might have altered the pituitary secretion of adrenocorticotropic hormone levels.
Another primary in-depth finding of the study relates to the change in the CRH and AVP ratio that influences the HPA functioning and AVP’s role-specific that affects the duration of HPA pulsatile hormone secretions among the OSA subjects.

ARE YOU OR YOUR LOVED ONES AFFECTED BY SLEEP APNEA?
Our process is designed using a patient-centered, holistic curative model that focuses on lowering costs while improving outcomes.
We serve veterans, minorities, families, and those who can’t get tests done at other facilities
Contrary Studies
Thanks to a recent study that has compiled almost all the contradictory research studies done so far. This publication claims that although a solid physiological link exists between the sleep-wake cycle and cortisol, a few studies failed to demonstrate the association between sleep quality and the concentration of cortisol levels in the blood.
Also, most studies neglect to analyze the relationship between sleep duration and cortisol levels. The publication also claimed that some research studies showed no significant association between sleep and HPA axis functioning, which contradicts all the research studies discussed above. This might have caused variations in age, sex, obesity, and the presence of any sleep disorder.
Specifically for OSA, experimental results exist that contrast the findings of other research studies. This research found no significant impact of OSA on HPA axis functioning.
Conclusion
Though sleep influences Cortisol’s blood concentrations more than the adrenocorticotropic hormone levels, the effect of sleep loss regulating the HPA axis functioning plays a vital role in controlling the secretion of adrenocorticotropic hormone levels in the body as per the circadian rhythm.
The regulation of adrenocorticotropic hormone becomes vital for your body to respond to stressful situations. If you follow the current and modern sleeping pattern (reduced or delayed sleep), the chances of getting diseases or disorders due to abnormal adrenocorticotropic hormone levels seem higher.
Hence, it becomes essential for you to check your sleep quality score now if you’re already a poor sleeper. On the other hand, healthy sleepers can still check their sleep quality score to improve their REM sleep.


