What do you know about Insulin? A hormone? Yes! And something that relates to blood glucose levels. Ninety-nine percent of the people knew only so much about Insulin.
But, in reality, Insulin does a lot of other crucial functions in your body apart from regulating blood glucose levels. It interferes with the carbohydrate, lipid, protein, and mineral metabolisms. Also, it intervenes in the functions of many tissues, organs, glands, and their hormones.
Did you know that nearly 7.4 million Americans have Diabetes (an insulin-related disorder) and take up Insulin supplements? If you’re one among them and wanted to know how to get your Diabetes reversed, continue reading this article. We’ve lined up the physiology (synthesis, function, and regulation) of Insulin, Insulin caused body problems, and how other factors like sleep and body weight can affect the Insulin levels in the body.
But, in reality, Insulin does a lot of other crucial functions in your body apart from regulating blood glucose levels. It interferes with the carbohydrate, lipid, protein, and mineral metabolisms. Also, it intervenes in the functions of many tissues, organs, glands, and their hormones.
Did you know that nearly 7.4 million Americans have Diabetes (an insulin-related disorder) and take up Insulin supplements? If you’re one among them and wanted to know how to get your Diabetes reversed, continue reading this article. We’ve lined up the physiology (synthesis, function, and regulation) of Insulin, Insulin caused body problems, and how other factors like sleep and body weight can affect the Insulin levels in the body.
Basics of Insulin
Insulin, a pancreatic hormone, plays a vital role in your human body to primarily regulate the circulating glucose levels in the bloodstream. The pancreas, located in a region behind the stomach, produces Insulin and releases into the bloodstream whenever needed.By regulating glucose levels, the insulin hormone enables the body cells and tissues to absorb instant energy (glucose), while also helping break down metabolisms like fat and protein breakdown.
Synthesis of the Insulin Hormone
There exists a cluster of cells called Beta cells in the Islets of Langerhans of the pancreas, which produces the insulin hormone. These beta cells become the primary source of the Insulin hormone in your human body. Insulin levels in the bloodstream decide the glucose levels that cells can absorb and use for respective metabolisms.The secretion of insulin by the beta cells can happen in two ways:
- Pulsatile: This release occurs only for the short term and gets utilized to absorb glucose from the blood.
- Protracted: This release occurs in the long term and gets utilized for major functions, including growth, cell division, protein synthesis, and DNA replication.
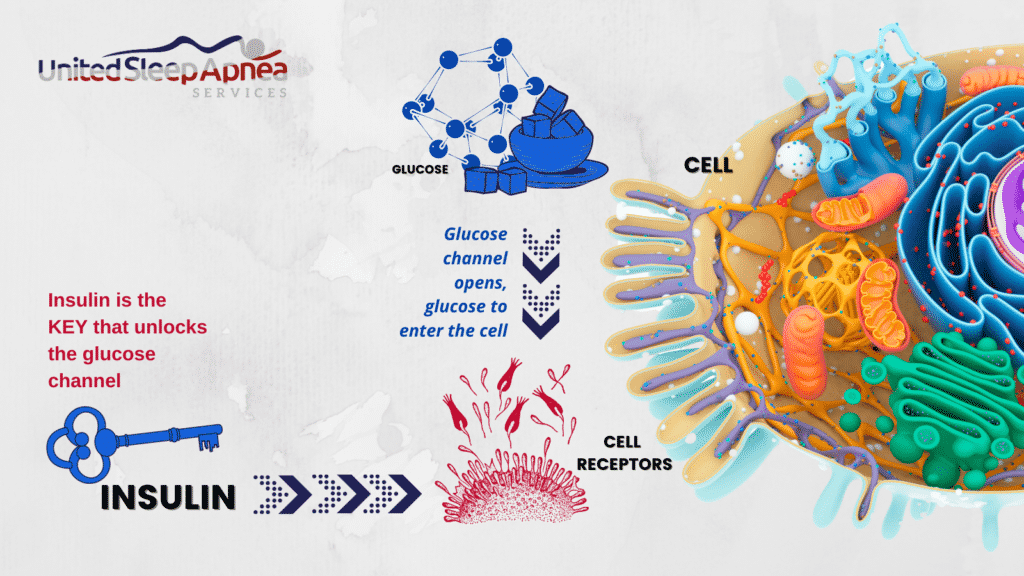
How does Insulin work?
Ideally, after you eat, the carbohydrates break down to release glucose. When glucose reaches the bloodstream, the insulin hormone gives the body cells a signal to absorb the glucose produced. Over time, in between the next meal, the insulin hormone signals the liver cells to store excess glucose when the glucose levels increase in the blood.The stored glucose can then get released when the blood glucose levels go down. In general, the more glucose levels, the more insulin activates.
The glucose released out of carbohydrate breakdown reaches the blood in the digestive tract initially, gets absorbed by the blood in the intestine, and then circulates throughout the body.
Key Functions of the Insulin Hormone
Regulating the glucose homeostasis throughout the body cells becomes the foremost function of the Insulin hormone. The two roles of stimulating glucose absorption and inhibiting gluconeogenesis constitute the functions of glucose homeostasis.A News Medical Life Sciences article discusses Insulin’s other functions:
- Stimulating glycogenesis and suppressing the glycogenolysis and gluconeogenesis in muscles and liver. This helps in the easy entry of glucose into muscles and adipose tissues.
- Storing excess glucose in the form of glycogen in the liver, thereby reducing the excess glucose levels in the bloodstream
- Modifying the activity of enzymes and enzymatic reactions
- Controlling the excretion of sodium in the urine
- Helping in breaking down protein and lipids in fat cells. This increases the amino acid (fatty acid) synthesis and absorption in muscle, liver, and adipose tissue. This also suppresses the breakdown of amino acids.
- As a metabolism, hindering lipolysis and enhancing lipogenesis/esterification
- Enhancing the brain functions in the memory aspects
- Helping in building up the muscles after injury and enhancing the strength of the muscles
- Helping in DNA replication
How is Insulin Synthesis regulated?
As the Insulin hormone plays a role in glucose regulation, glucose serves as the primary regulator. Thus, glucose metabolism plays a key role in controlling Insulin hormone synthesis via a specified transcription and translation process.A research publication (2013) in Current Diabetes Reviews studies in-detail the regulation of insulin synthesis and secretion.
The study reveals how the pancreas’ beta cells react to blood glucose concentrations via capillary action (small pores called fenestrae. Without fenestrae, the permeability may get reduced, and beta cells cannot quickly sense the glucose concentrations.
Other key regulators include amino acids, fatty acids, and a bunch of hormones.
- Amino acids: Glutamine, together with leucine, stimulates insulin secretion by inducing the GSIS (Glucose-stimulated Insulin Secretion) process by the beta cells.
- Fatty acids: Beta cells of the pancreas possess free fatty acid receptors (FFAR -1) that may aid in insulin synthesis and secretion.
- Hormones:
- Melatonin: Studies claim that melatonin hormone has multiple (Stimulation, Inhibition, and sometimes Neutral) regulatory reactions over insulin synthesis.
- Leptin: This inhibits insulin secretion and suppresses the role of insulin in fat and liver tissues.
- Estrogen: The 17β-estradiol increases insulin secretion.
- Growth hormone: Stimulates the production of insulin-like growth factor-I (IGF-I) and its binding proteins
- Incretin: GLP-1 stimulates insulin secretion after nutrient intake.
A 2014 study on Insulin structure and structure-related functions unveiled that Insulin regulation also associates with a set of events involving plasma membrane depolarization and calcium-ion homeostasis.
Effects of Altered Insulin Sensitivity
Problems arise when your body does not produce enough insulin or cells do not absorb enough insulin. In this case, when insulin cannot perform its functions, then imbalanced blood glucose levels may affect other body functions, including vision (eyes), cardiovascular roles (heart), signaling (nerves), and filtration (kidneys).Insulin Deficiency
Diabetes mellitus persists very commonly today and arises due to insulin deficiency. The types of Diabetes include,- Insulin-dependent Diabetes mellitus (Type 1): This condition arises when the beta cells’ insulin production does not suffice the need to regulate blood sugar (glucose) levels. In this case, there might be inflammation or destruction in beta cells of islets of Langerhans. The symptoms include increased thirst, frequent urination, blurred vision, unexpected weight loss, extreme hunger, and frequent mood changes.
- Non-insulin-dependent Diabetes mellitus (Type 2): This condition arises when insulin does not effectively carry out its glucose regulation functions. Mostly, people with obesity have this type of Diabetes. In this case, the patient’s beta cells fail to produce enough insulin to overcome insulin resistance. The symptoms include slow healing of external inflammation (wounds), numbness, dark skin patches, extreme tiredness, and tingling.
Insulin Excess
Elevated Insulin secretion leads to Hyperinsulinemia. Insulin-secreting tumor cells called insulinoma cells develop in the pancreas, causing excess synthesis and secretion of Insulin. When a human brain faces hormone shock (insulin shock) due to excess secretion, it might lead to survival or life-threatening consequences.Hyperglycemia
When insulin sensitivity or activity decreases, the blood glucose level does not get controlled, leading to Hyperglycemia. Increased thirst resulting in frequent urination becomes one of the major symptoms of this condition.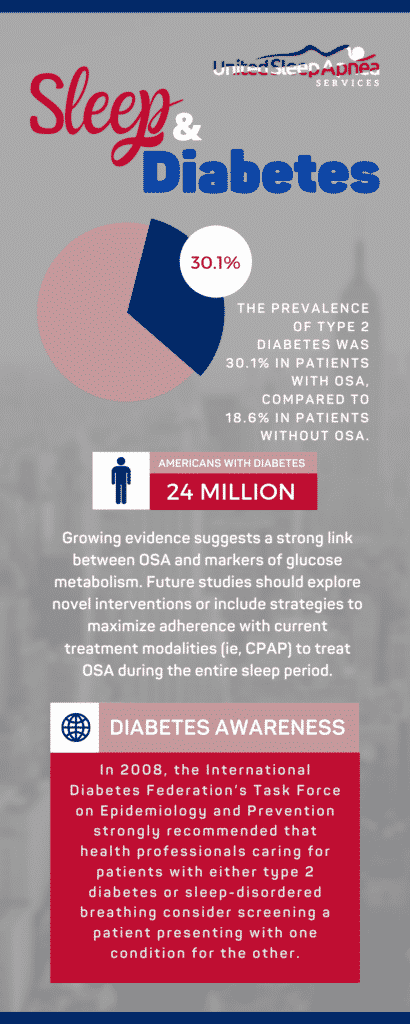
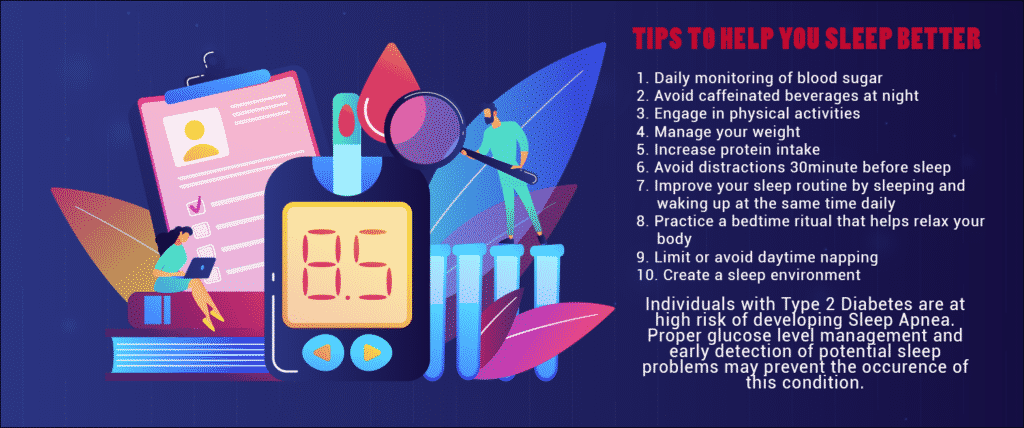
Does Sleep Affect Insulin Levels?
In simple biology, higher cortisol is secreted in individuals with poor sleep, thereby hindering insulin function. Sleeping disorders like sleep apnea seem to elevate the individual’s risk of getting Diabetes.An article published by Sleep Foundation gives an overview of the association between insulin and sleep. The article claims, with consistent sleep deprivation, the insulin secreted does not suffice to balance the blood glucose levels. And hence, the stress hormone (Cortisol) and other hormones (Thyroid-stimulating hormones and growth hormones) get activated, which keeps you awake for longer. This results in increased blood sugar and a higher risk of Type 2 Diabetes. In particular, the slow-wave (deep) sleep, when lost, affects insulin sensitivity and fails to control the blood sugar.
When they carried out studies involving 4,000 people, researchers found that individuals who experienced poor sleep (less than 6 hours) had less insulin sensitivity and higher chances of developing Diabetes.
Also, during sleep, all the metabolic functions start reducing, thus reducing the need for glucose (instant energy). When insulin does not control the blood glucose levels, it affects all other functions from signaling hormone synthesis.
Experimental Studies
An article (2019) published in WebMD claims that insulin can perform its function even if the blood sugar levels increase at midnight. However, with Diabetic people, their insulin becomes incapable of handling the nocturnal peaks of blood sugar.A 2014 study published in the Endocrinology and Metabolism Clinics of North America showed that insulin secretion peaked after food intake, irrespective of the time of the day (Day or nocturnal). And the levels decreased during sleep. The researchers also found that sleep deprivation resulted in a significant increase in insulin resistance.
A Healthline article supports this finding and confirms that lack of sleep induces Type 2 Diabetes.
Sleep Apnea and Insulin
Obstructive sleep apnea, a sleep fragmentation disorder, hinders patients’ sleep and makes them wake up frequently, affecting the circadian and pulsatile release of hormones.A research study published in the journal of Endocrinology and Metabolism Clinics of North America infers that people with obstructive sleep apnea exhibit decreased insulin activity and increased cortisol activity.
Regardless of the above research findings, a study observed unique findings that sleep disorders like obstructive sleep apnea do not affect insulin sensitivity. The study also found that weight gain (obesity) significantly contributed to the changes in insulin sensitivity. Another important factor that associates with insulin sensitivity includes oxygen saturation. The research also studied in-depth the effect of central obesity on insulin resistance via increased fatty acid circulation and lipolysis.
A research publication released in the journal of Diabetes Spectrum in the year 2016 shows that obstructive sleep apnea increases Type 2 Diabetes risk, irrespective of the subject’s age and weight factors. However, obesity has become one of the main risk factors for both Diabetes and obstructive sleep apnea. The research also claims that early diagnosis of obstructive sleep apnea can help restore insulin activity and prevent further insulin-related diseases or disorders, including hyperglycemia.
Can Diabetes affect your sleep quality?
A recent publication (2018) in the Sleep Doctor Forum claims that sleep disruption increases with the presence of diabetes. Also, individuals with diabetes had higher chances of developing sleep apnea, a kind of sleeping disorder.The publication also mentions that according to the CDC (Centers for Disease Control, USA), more than 100 million individuals in American suffer from Diabetes or Prediabetes. And more than one-third of them face challenges in healthy sleeping (7 hours and above).
Taking Insulin shots?
When sleep affects insulin secretion and people with Diabetes develop sleeping disorders, it creates a significant need to test and analyze an individual’s insulin levels and sleep quality regularly. Research scientists have found that diabetic people with poor sleep have 82% chances of developing increased insulin resistance than healthy sleepers with diabetes.Also, statistics released in the UChicago Medicine shows that people who slept less (poor sleepers) had higher blood sugar levels (around 23%) and higher insulin levels (around 48%).
If poor sleep caused diabetes in your case, you might get out of danger, and your Diabetes could reverse! Yes, scientists have provided confidence that if you have experienced sleep loss only for a short period and if the healthy sleep retains sooner, then your Diabetes can get reversed.