The Basics of Bone
Bones become the vital and dynamic structured compositions of a human body. The primary function of a bone includes locomotion (allowing us to move from one place to another) and protection. With its framework of connecting tissues, bones enable your body’s muscles and various organs to obtain a rigid placement.
In normal conditions, the short, long, and irregular bones in your skeletal system form via endochondral ossification, the process by which growing cartilage is systematically replaced by bone to form the growing skeleton. Whereas, the flat bones of your skull, face, and pelvis form via intramembranous ossification, which is the direct conversion of mesenchymal tissue into bone.
Bone Metabolism
The metabolism of human bone follows a continual cycle or a complex sequence of bone growth and resorption. Bone growth results in the formation of bone cells by a process called Osteoblastogenesis
(Os-Tee-O-Blas-Toe-Genesis). Bone resorption results in the breaking of bone cells by a process called Osteoclastogenesis. Osteoblasts, Osteoclasts, a set of hormones, and other influencing factors catalyze this cycle of bone formation and bone resorption in the human body.
The properties of bone metabolism include bone mass and bone loss. Both bone mass and loss state the measurement of mineralized bone tissues in your body by volume, size, and density. Sleep and bone health go hand in hand. Let us explain:
– Bone mass: In general, humans meet the peak bone mass between the ages of 16 to 25.
– Bone loss: The structural and various metabolic factors alter the rate of loss in humans. In general, bone loss occurs at a rate of 0.3% to 0.5% every year. For menopausal women, the rate increases drastically.
Composition of Bone
The cellular components, the extracellular matrix, and water constitute the human bone composition.
- The cellular components comprise of Osteoblasts, Osteocytes, and Osteoclasts cells.
- The extracellular matrix comprises organic and inorganic components.
- Organic components include collagen type I and non-collagenous proteins.
- Non-organic components include calcium phosphate minerals.
 Functions of Bone
Functions of Bone
- Provides mechanical support to muscles and tissues
- Protects the bone marrow from any damages
- Responsible for body movements by acting as point and levers
- Acts as a reservoir for calcium, phosphates, and other minerals
- Acts as a cage to protect the internal organs from any injury
- Hosts the production of blood cells within the marrow (Red marrow)
- Serves as energy reservoirs (Yellow marrow)
The Bone Metabolism of Modeling and Remodeling
The dynamic cycle of bone formation and resorption occurs throughout the life of a human body. The cycle plays a vital role in making your body adapt to growth (form or structural changes) and mechanical forces. At equilibrium, the intensity of bone formation (bone modeling) equals the bone resorption (bone remodeling). The specialty of bone metabolism lies in the integrity of this equilibrium (bone modeling and remodeling).
Until the growth, both the intensities equal each other following a sequence of modeling and remodeling. But, once your body attains the peak bone mass (between the age of 16 – 25), the intensity of resorption increases than that of the formation.
The bone metabolism cycle divides into three stages:
- Initiation of an impulse: Nothing but a mechanical load or stimuli
- Bone resorption by osteoclasts: Hematopoietic cells produce osteoclast cells that contain proteolytic enzymes, acid phosphatase isoenzyme, and calcitonin receptors. Signals from osteoblasts control the activity of these cells, and its primary function includes bone resorption.
- Bone formation by osteoblasts: The bone marrow’s mesenchymal cells produce osteoblast that involves proteo-synthetic activity and contains alkaline phosphatase, calcitriol, and growth hormone receptors. Bone cell formation, bone mineralization, and maturation management constitute the primary function of these cells.
Do you want to explore similar comprehensive knowledge pieces? Follow us on Facebook, Pinterest, Twitter, and Instagram
Regulation of Bone Metabolism
The regulation of the bone metabolism cycle proceeds by a complex interlining of systemic hormones, other local factoring substances, and biochemical markers.
The hormones can be of two types:
- Hormones that affect calcium phosphate metabolism:
- Calcitriol, parathormone, and calcitonin carry out the regulation of calcium-phosphate metabolism.
- Parathormone: It increases the activity of osteoclasts and stimulates the bone resorption process. This increases the secretion of calcium and phosphates from the bone to your bloodstream.
- Calcitriol: It helps in the photosynthesis activity, enabling the increased absorption of calcium and phosphates. This results in collagen formation, leading to healthy bone formation.
- Calcitonin: It inhibits the activity of osteoclasts and reduces the intensity of the bone resorption process. Thus, accumulation of calcium happens in the bone.
- Hormones that affect other metabolisms:
- Insulin: It induces the activity of osteoblasts and respective modeling/remodeling functions.
- Estrogens: The functions of estrogens resemble the functions of calcitonin. Hence, they involve in the inhibition of bone resorption and stimulation of bone formation.
- Glucocorticoids: It inhibits protein synthesis by osteoblasts and paves the way to osteoclasts. This reduces the intensity of bone formation.
- Growth hormone: This hormone produces insulin-like growth factors (IGF 1 and 2) to stimulate bone formation.
- Thyroid hormones: It stimulates the activity of osteoclasts, and thus helps in bone resorption.
Local factoring substances include:
- Insulin-like growth factor 1 (IGF-1): Stimulates osteoblasts
- Platelet-derived growth factor (PDGF): Stimulates osteoblasts
- Fibroblast growth factor (FGF): Stimulates osteoblasts
- Interleukins (IL-1, IL-6, etc.): Stimulates osteoclasts
- M-Colony stimulating factor (M-CSF): Stimulates osteoclasts
- Interferons (INF-γ): Stimulates osteoclasts
- Bone morphogenic factor (BMF): Stimulates osteoblasts
Biochemical markers include:
- Bone formation markers: Alkaline phosphatase, serum osteocalcin, and Terminal peptides of procollagen type I
- Bone resorption markers: Acid phosphatase, Urinary deoxypyridinoline, and Carboxy-terminal telopeptides of collagen
Bone Metabolism Disorders
As the name suggests, in osteoporosis, the patients’ bones become porous than normal conditions, making them thin, weak, and lighter. This increases their risk of getting fractured, even with slower or mild stress.
Very commonly, women at the menopausal stage experience increased bone loss mechanisms. This increases their chances of osteoporosis significantly than usual. Research and industry experts predicted that one-fourth of the world’s women population (above 60 years of age) has a higher probability of getting this bone metabolism disorder.
The long, short, and irregular bones in your skeletal system follow the bone formation via endochondral bone ossification. When this endochondral bone ossification process gets disturbed, it leads to rickets. In these patients, improper mineralization of osteoid tissue leads to increased accumulation of the organic matrix.
When rickets affects children, they show deformities in the skull, thorax, and leg bones formation.
In general, the lack of vitamin D leads to rickets in children and osteomalacia in adults. The osteomalacic patients suffer from weakened bones due to which they also face bone pain, numbness, and increased chances of bone fractures. The bone mineralization in these patients may have gone deficient due to improper absorption of minerals or lack of enough sunlight or vitamin D deficiency.
This disorder arises when your bones cannot lose its ability to withstand a usual or normal load, even being denser. The affected bones lead to hyperactivation of osteoclasts and cause severe pain and neurological problems. The X-ray method helps in diagnosing this disorder.
Osteogenesis Imperfecta (Brittle Bone Disease)
One of the genetic disorders of bone metabolism, osteogenesis imperfecta, occurs due to the defective gene of collagen type I. When collagen, the bone-strengthening component, becomes defective, the bones naturally lose its robustness, leading to the formation of fragile bones throughout your body.
In some cases, the patients may undergo only a few fractures throughout their lifetime. But, in special cases, patients may undergo hundreds of fractures.
 How lack of sleep affects your bones?
How lack of sleep affects your bones?
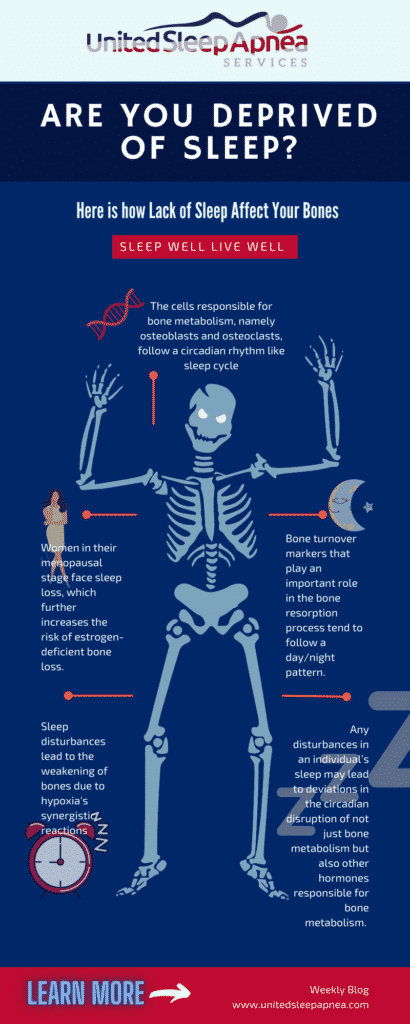
In humans, the normal sleep cycle follows a circadian rhythm. Also, the pulsatility of a few hormones like Cortisol and Human growth hormone happens in line with this rhythm. Likewise, the cells responsible for bone metabolism, namely osteoblasts and osteoclasts, also seem to show the circadian rhythm.
Bone turnover markers that play an important role in the bone resorption process tend to follow a day/night pattern. The release of such markers of bone resorption increases overnight and attains its peak in the early morning (REM sleep). The release gets reduced gradually until late afternoon.
Hence, any disturbances in an individual’s sleep from things such as sleep apnea or other sleep disorders, contribute to a higher nocturnal light exposure which may lead to deviations in the circadian disruption of not just bone metabolism directly but also other hormone secretions and metabolisms that can inadvertently come full swing back to your bone metabolism.
Research studies that deal with the association of sleep disturbances with lower bone mass among the elderly showed increased morbidity and mortality problems.
Also, women in their menopausal stage face sleep loss, which further increases the risk of estrogen-deficient bone loss.
Association between Sleep Apnea and Bone Metabolism
In the U.S., adults and the elderly (above 50 years) exhibit consistent sleep disturbances. Obstructive sleep apnea (OSA) ranks first in the most common sleep-disordered breathing problem in the U.S.
In the U.S., adults and the elderly (above 50 years) exhibit consistent sleep disturbances. Obstructive sleep apnea (OSA) ranks first in the most common sleep-disordered breathing problem in the U.S.
Researchers link obstructive sleep apnea with an increased risk of improper bone metabolism and higher chances of osteoporosis. Studies have already found the association of OSA with obesity, high blood pressure, cardiovascular diseases, and depression just to name a few. Besides, the association of OSA with bone metabolism creates higher demand to treat the problem at earlier stages in both children and adults.
When OSA characterizes a cycled sequence of hypopnea and hypoxia in tissues, this might also affect the bone metabolism at a higher pace. Also, when sleep apnea begins to constantly deprive the oxygen levels, it can probably lead to weakened bones and a higher risk of osteoporosis. When these conditions continue for a longer period, the patient may become prone to severe bone fractures, weakened bones, reduced quality of life, and sometimes death.
Another research carried out in Taiwan showed that people who suffered from OSA demonstrated 2.7x higher chances of developing osteoporosis.
Symptoms of obstructive sleep apnea include restlessness, crampy feeling, morning headaches, depression, daytime drowsiness, lack of focus/concentration, and snoring.
Direct Effects of Sleep Apnea on Bone Metabolism
The episodes of hypoxia in OSA may lead to ischemic injury that creates an acidotic microenvironment in bones. This affects the family of transcription factors like Hypoxia-Inducible Factor (HIF) that regulates bone metabolism.
Sleep disturbances, including sleep fragmentation and insufficient sleep over a longer period, lead to the weakening of bones due to hypoxia’s synergistic reactions.
Insomnia with poor sleep quality has also been found to show some association with increased risk of osteoporosis.
Indirect Effects of Sleep Apnea on Bone Metabolism
The direct effects of sleep disorders (Insomnia, OSA, Hypoxia) with bone metabolism greatly differ from that of the indirect effects of sleep apnea on bone metabolism. It happens through associated medical problems like insulin resistance, vitamin D deficiency, cognitive disability, obesity, and hypogonadism.
Some indirect reactions that sleep apnea initiates include:
- Insulin resistance
- Growth hormone suppression
- Osteoclasts stimulation
- Osteoblasts suppression
Conclusion
Desynchrony in any circadian rhythms or sleep patterns in your human body induces a lot of metabolism-related issues. But, the effect and the potentiality of the effects that it causes to bone metabolism in an individual depends on age, gender, life stages, innate sleep cycle, and quality of bone remodeling/modeling.
Take up the Epworth Sleep Scale test now and let us join you on your journey to a better nights’ sleep! Sleep Dreams!


